Or
Why health technology is more exciting than electronic patient records
By Peggy Salvatore MBA
*Definition 1: An area of muddy or boggy ground. Definition 2: A complicated or confused situation.
For many years, the promise of electronic patient records pointed to the promise of massively improved health through better information about the patients in front of us and all the data on the back end for research. And then we got implementation, or some highly regulated and fragmented version of it, that resulted in sometimes even less valuable information at the point of care today than when system implementation began.
How could that happen? Easily enough. The software took center stage, and with it all the training, technical, regulatory, security and work process issues that took the focus off patient health. Instead of more health, electronic patient records led to more administrative tasks.
Here’s the proof. In just the last week, my health news inbox was brimming with
- warnings about ICD-10’s looming deadline ,
- the challenges of meeting Meaningful Use 2
- the unresolved vision for Meaningful Use 3,
- a deadline for the latest reporting form (IRS Form 1095-C) for employers with more than one employee regarding compliance with the ACA ,
- penalties for not meeting ACO outcomes metrics , and then
- a very enlightening article posted by Dr. Edward J. Schloss who has determined that electronic health records mostly serve to meet regulatory requirements with almost no utility for the patient’s health or malpractice information for the lawyers
The Promise vs. The Reality of Electronic Patient Records
The above news about healthcare measurements, payments, penalties and documentation scream that today the electronic patient record is all about the administration of healthcare. If you are a provider and you deliver service, your primary concern when you engage with the electronic patient record is getting paid, not getting fined, getting outcomes that line up with pre-determined, government-sanctioned measurements and staying out of jail. Then, if you have any energy left over, you can consider what disease the patient in front of you has and how to best treat it within the confines of getting paid, not getting fined for not getting outcomes that line up with pre-determined measures and staying out of jail.
Whew!
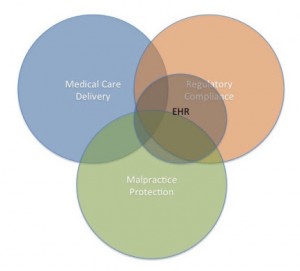
No wonder that Dr. Edward J. Schloss sat down and did a Venn diagram about the true value of the electronic health record. In his analysis, in his doctorly and very scientific way, he drew a picture of the value of an EHR which showed that most of its value lies in its ability to help providers adhere to regulations. You can go here to his blog to read his entire analysis.
So much for the promise of the electronic patient record. As originally conceived, it would help create a great and accurate documentation trail so patients and their care team could have a complete picture of the patient’s health status and treatment history. It would capture disease states and treatment outcomes for research. We’d know which treatments and procedures worked in which patients and under what circumstances. With all this information, future patient diagnoses would be quicker and more accurate, the best treatment faster and more effective.
The reality? The record’s best and highest use as currently designed is to make sure providers capture the data that regulators deem important, that payers need to justify payment, that doctors need to document to avoid fines and malpractice suits, all secured in a way to keep you HIPAA-compliant and out of jail.
The promise was great and the reality is depressing.
The Promise of Health Technology
The best of the future lies in technological advances, with technology defined as applied science. Since electronic patient record documentation is going down a dark alley right now, where health technology is going is much more exciting. The promise of diagnostic tech, treatment biotech, and health tracking apps point in the direction of health care.
Every day you can read about more than one exciting startup that has developed a new app to monitor performance and function, or some new discovery in the lab that promise cures for Alzheimer’s Disease and Parkinson’s. This week, Peter Diamandis’ and Ray Kurzweil’s Singularity University student competition funded a startup called MirOculus.
Here’s the scoop from Diamandis:
MirOculus: MirOculus is creating a simple blood test that can tell you, at the molecular level, the exact type of disease you have and its severity before it presents any symptoms, and then monitor the success of the treatment. They are also focused on cancer detection using microRNA biomarkers, leading to routine cancer screenings that will allow for early-stage detection and the prevention of millions of cancer deaths.
As venture capital turns more toward health, the integration of these new technologies into a patient’s historical and treatment electronic record can be truly helpful. If only we can keep the regulators from regulating the promise out of the promising application of health technology, too.
As Diamandis said in his September 7 newsletter: “Healthcare is so massively broken, that its disruption will come easy and happen fast.”
Looks like that is happening right now.