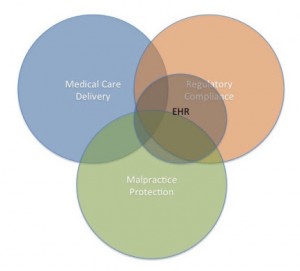
Last week’s blog explored the relationship between collection of patient data and value-based payment for patient outcomes. The fact that payments will be driven by data is one of the lesser recognized drivers of data collection, but it is of no small consequence to providers. Ultimately, if accountable care organizations (ACO) manifest as planned, integrated health networks will be paid for performance based on a defined set of quality indicators as evidenced by the data.
Provider organizations are gearing up for the switch, and a fully functional electronic patient record system is an integral part of a viable ACO. Performance-based payments mean that the fee-for-service model will become rare, perhaps extinct. When providers are paid, not by each incident of service or each product/treatment prescribed, it will necessarily drive down the cost of individual products and services since they will not be reimbursable at cost. In fact, their reimbursement will not be assured since payment will be based on retrospective data.
Patient’s Right to Most Effective Treatment
I was speaking with a cardiologist about the effect that performance-based pricing has on his patients, and his most notable complaint was that he felt the patient has no rights in this lowest bidder environment. His typical case in point: It sometimes takes a year or more to find the right combination of drugs to control a patient’s heart condition. He usually determines an effective therapeutic regimen after lengthy trial and error. If, however, the patient changes jobs or the patient’s employer changes health plans, often the drug formulary changes with it and the preferred drugs on the new formulary are not in the patient’s regimen. Formularies are a form of performance-based pricing since a health plan must be convinced by the pharmaceutical companies that particular drugs will work and the plan will recoup its costs in healthier patients. If a patient becomes subject to a new drug formulary, at that time, the cardiologist can either spend time and effort attempting to establish medical need of the patient’s regimen by filling out paperwork and going through an appeals process, or he has to attempt to find new treatments covered by the new plan and another period of trial and error commences.
This physician was passionate about this issue and how it has negatively impacted his patients. He suggested that a Patient’s Bill of Rights needs to be implemented as part of the national overhaul of healthcare to protect patient care. In his example of pharmaceutical coverage, he would like to see his patients who are controlled on specific medications to have the right to continue on those medications even if the payer changes.
When we think about HIPAA today, we think about the patient privacy elements of that law. But very clearly, the Health Insurance Portability and Accountability Act of 1996 was also about the portability of insurance – that patients had the right to take their health insurance with them so they wouldn’t have coverage interruption if they changed jobs. Much of this concern has been made moot by ObamaCare that can kick in whenever someone doesn’t have coverage. Piggybacking on the concept of portability of health insurance, the cardiologist is suggesting that patients also have the right to continue effective care from one provider and payer to another.
Lowest-Bidder Healthcare
Imagine, if you will, that as all pharmaceuticals, treatments and diagnostics enter the system of performance-based payments, they will no longer be paid on an as-needed, per unit basis but rather as part of a lowest-bidder system. Already, I saw an article today encouraging labs and pathologists to rethink their pricing structure to accommodate the ACO model. The underlying message was that they will need to move from the current fee-for-service structure to one that provides package pricing at bottom-feeder rates to compete for the business of hospitals and health systems that are being driven into this outcomes-based reimbursement scheme.
As we move toward outcomes-based payment models, no part of the health care system will go untouched. Everyone will be forced into a “value” proposition payment model and that means patients will be driven toward certain low-cost providers, treatments and labs.
Which leads to this cardiologist’s concern. Will patients have any rights to choose their drugs, their providers, their labs or really any part of their healthcare that they prefer or works best for them individually? Or will they be driven into a uniform system of treatments and providers based on best value for the price as determined by the data?
Perhaps resurrecting the idea of a Patient’s Bill of Rights would act as a countervailing force in this lowest bidder scenario.